How genetic therapies transformed the lives of sickle cell patients
Their stories are divided into before and after.
First, those long years of pain which flooded every moment -- school, relationships, work.
And then -- after agonizing treatments -- what felt like the miracle of life after sickle cell disease (SCD).
Two Americans whose lives were turned around by newly approved treatments tell AFP they want others to benefit too.
But the eye-watering cost -- up to $3.1 million per course of treatment -- could limit access for other patients.
- 'Like coming to life' -
Tesha Samuels was born in 1982 -- just before the invention of prenatal screening for SCD, an inherited red blood cell disorder.
SCD affects around 100,000 people in the United States and some 20 million worldwide.
Most people with the condition are Black. Scientists say this is because the sickle cell trait evolved to protect people exposed to malaria, so the risk of SCD is higher.
Those with the disease have abnormal hemoglobin -- the molecule that carries oxygen -- making their red cells hard and C-shaped like sickles.
Complications include anemia, bouts of extreme pain, organ damage and early death.
Tesha was diagnosed aged two and recalls a childhood in and out of hospital.
At seven, she suffered a life-threatening case of anemia and then aged 13 she had a stroke which led to monthly blood infusions.
Tesha said "the stigma of a Black child going to the hospital saying they're in pain" made her wait until things got unbearable.
As a young adult, Tesha saw the disease take the life of a dear friend named Mohammed, a fellow "sickle cell warrior" who would often end up in the same hospital as her.
She began studying at the prestigious Howard University hoping to become a doctor but her health forced her to drop out. She then tried community college but, once more, SCD meant couldn't finish.
"You downgrade your dreams based on your capacity in sickle cell," said Tesha.
As a newlywed in her twenties, she was dismayed at needing an intravenous medicine drip for eight hours every night to manage her condition.
But in 2018 her life turned a corner when she became one of the first ever people to receive an experimental gene therapy.
The procedure -- now marketed as Lyfgenia -- uses a modified virus to deliver a functional version of the hemoglobin-producing gene. .
First, doctors draw out stem cells from the bone marrow before modifying them in a lab. Then comes the hardest part -- chemotherapy to clear the way for the return of the treated cells.
In addition to losing all her hair, chemotherapy saw Tesha have a 16-hour nosebleed which left her in intensive care.
Her recovery was further complicated as her blood platelets, which are essential for blood clotting, took months to bounce back.
But when they did, her energy levels soared.
"It's almost like coming to life," Tesha said. "Here's this new life ahead of you. What do I want to do with it?"
Tesha went back to school to complete her degree.
She also started her own advocacy group, Journey to ExSCellence, to spread word of the treatment among the Black community.
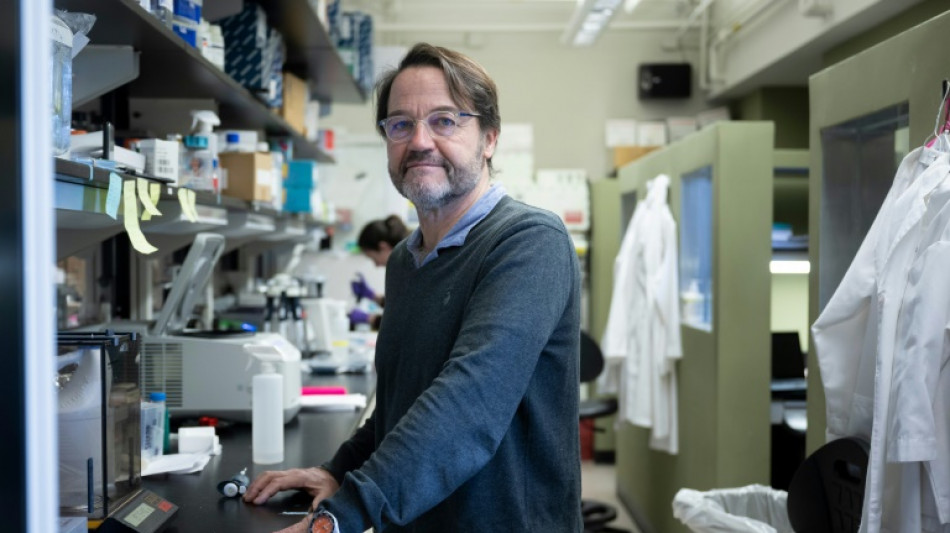
"It looks like the cure, but we like to call this 'transformative,'" said physician-scientist John Tisdale of the National Institutes of Health, which ran the trial Tesha took part in.
Tisdale emphasized that each patient needed monitoring for 15 years to complete the study.
- Childhood struggle -
Jimi Olaghere's first memory of sickle cell goes back to when he was eight-years-old, playing soccer with other kids in his native Nigeria and needing to stop every five minutes for rest and water.
"I asked my mom, why am I different?" he remembers.
His parents sent him to live with his aunt in New Jersey where there was better health care but his childhood remained a struggle.
Jimi, 38, was unable to complete college and found his disease was too heavy a burden to place on most romantic partners, until he found his wife who was willing to embrace the challenge.
The disease also took a terrible toll.
His gallbladder was removed, he had a heart attack and lung clots. At his worst, he recalls spending 80 percent of his time in bed.
Moving to the warmer climate of Atlanta brought some relief, as it does for many with SCD.
Then, in 2019, he heard about a CRISPR gene therapy clinical trial. He applied to be tested for eligibility and received a "magical" voicemail telling him he was in.
Thanks to the CRISPR-modified stem cell therapy he received, now marketed as Casgevy, Jimi is "basically living the dream now."
He has three children, thanks to IVF, and runs several small businesses.
Like Tesha, Jimi has raised his voice to advocate for others, particularly in Africa, where access to such treatment seems a far-off dream.
Tisdale, of the NIH, said the next step was reducing the physical burden of the treatment and making it cheaper.
It remains unclear how much private insurers will pay to offset the procedure's enormous costs.
But Medicaid, a US government-backed insurance program, has said it will pay for the therapies starting next year.
D.Gallaugher--NG



